Intubation, Ventilators and Tracheostomies
So just to warn you I've never been trained in the actual intubation process (not an EMT or a provider), I've had to do some research for the actual process. Thus I've done research on the matter but if something is a little off I'm afraid I won't necessarily know it.
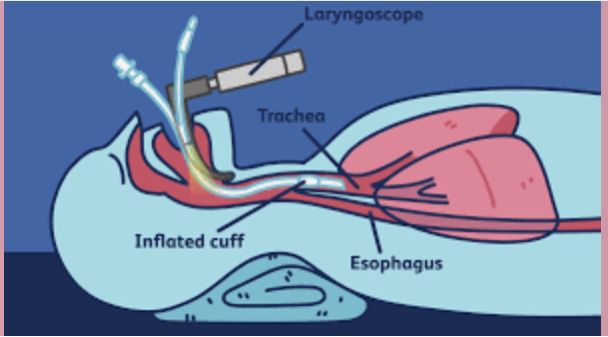
Intubation helps keep the airway patent (open) when, for whatever reason, a person can't maintain the airway on their own. This video helps describe the process. The man's voice is a bit monotonous but the info is still good. The first couple minutes gives a quick snapshot of the anatomy and physiology of the lungs, whereas the intubation process itself starts to be explained at 3:12.
[There should be a GIF or video here. Update the app now to see it.]
Ideally a person is sedated or unconscious when intubation happens, but in emergency situations that might not always be the case.
If the tube has gone down the esophagus the lower abdomen will rise and fall with the artificial breaths rather than the chest. The tube needs to be withdrawn quickly because, while air in the stomach is not quite an emergency that a feeding tube in the lungs is, the stomach was not made to be full of air. As mentioned in the video the gold standard to confirm placement is an x-ray.
The tube is then secured to the person's cheek to prevent displacement. It's extremely anxiety-inducing to not be able to breathe in one's own power. and having the tube down the trachea commonly causes a feeling of suffocation. Additionally, due to the inflated cuff keeping the tube in place, the person is unable to talk which can also increase anxiety. These factors, combined with underlying trauma or disease processes that caused the need for a ventilator in the first place, often result in the people on ventilators being kept moderately sedated, and occasionally the use of soft wrist restraints.
Ventilators
There are different ventilator settings. The most well known is the settings that completely take over breathing for the person. Another setting (SIMV) allows people to take their own breaths, only stepping in if the person is breathing too shallowly or infrequently. Some settings just help keep the airway open by providing positive pressure in the airway (PEEP- which is similar to how a CPAP machine works).

Being on a ventilator requires immobility to maintain tube placement. In addition to the risks described in my earlier chapter on immobility, people on ventilators are at high risk for pneumonia. Keeping the head of the bed elevated, frequent oral care and proper suctioning can decrease this risk. They're also at risk for pneumothorax (air in the chest cavity) if the air pressure becomes too much for the lungs. Then the need for a chest tube might come into play. People are also at risk for malnutrition because they're unable to eat orally. TPN (nutrients through and IV) or a surgically placed gastric tube are often used to help prevent this.
With prolonged use of ventilators people will need to be weaned off because it doesn't take long for muscles to get lazy. A person will likely have 'sedation breaks' where medications aren't given so as to see how effective the person is breathing on their own.
Some people end up being on ventilators the rest of their lives, but these are more likely to be connected to trachs than from indwelling tubes. I personally have worked with home health clients who had ventilators in their own homes.
Trachs
A tracheostomy is a hole in a person's throat, held open by a small tube. This happens when the airway is compromised and needs to be held open.

A trach may be short term or permanent, hooked up to a ventilator or contingent on the person's own breaths. Depending on the person's condition the trach can be where they both inhale and exhale, or just where they inhale. Special 'plugs' known as speech valves (the purple cap pictured below) allow air in, but doesn't allow air out (forcing the person to exhale through their mouth) which allows air to pass through the vocal cords. The movement of air means the person can talk, and this method can also help train a person to breathe through their mouth again.
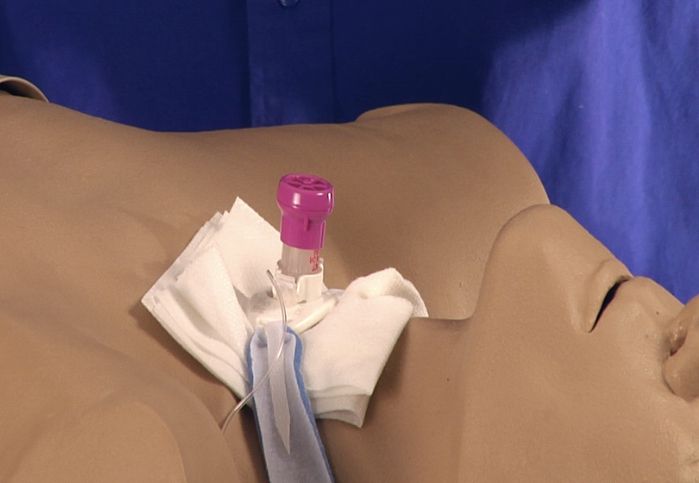
How often trachs need to be cleaned varies somewhat from person to person. Phlegm develops around the stoma (hole) and within the tube itself that needs to be suctioned out since the person is unable to cough. Suctioning can be every five minutes to once a day. The skin around the throat needs to be cleaned at least daily to decrease risk of skin breakdown and get rid of the secretions.
If a trach, especially a new one, becomes dislodged or falls out (decannulation) this is an emergency. The body recognizes the stoma as a wound that needs to be closed. It can be as few as minutes for the trachea to constrict enough that the initial trach doesn't fit anymore. For this reason most people on trachs have an extra cannula (tube), typically 2, within easy reach; one that is the same size they currently have in their trachea, and one the next size smaller. Some people might do okay without it, depending on their condition, but if proper action is not done quickly a person can easily go into respiratory distress after decannulation.
Bạn đang đọc truyện trên: AzTruyen.Top